Cartilage Repair
ARTICULAR CARTILAGE LESIONS | SURGICAL OPTIONS FOR BIOLOGIC RESURFACING
ARTICULAR CARTILAGE LESIONS
OsteoArthritis: Your Choices & Future
As the articular cartilage surfaces breaks down and degenerates in a joint, it can cause pain, stiffness and swelling. This is called arthritis (osteoarthritis, degenerative arthritis) and is most common in the hand and knee with some 30+ million Americans having some form of this “wear and tear” arthritis.
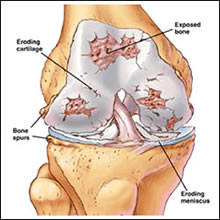
Figure 1 – Osteoarthritis

Figure 1 – Osteoarthritis Photo
Often it can come from trauma and generally arthritis increases with age. There is a hereditary component. Arthritis is treated by weight reduction, activity restriction, NSAID’s (nonsteroidal anti-inflammatory drugs) like aspirin, Motrin, Alleve, Celebrex (not Vioxx anymore), Indocin, etc. Plain Tylenol can help relieve the pain. Exercise is also important to keep the involved joint loose and less stiff. Muscle strengthening around the arthritic joint is also helpful. Surgery to smooth or trim rough arthritis surfaces is usually not beneficial.
Occasionally, localized defects in the cartilage can be treated with different surgeries to fill this defect in the knee. This can help relieve pain and protect the joint over time to slow down the progressive destruction of the joint surface. My approach is always to provide a biologic surgical alternative to the damaged cartilage surface. This can hopefully provide my patients with “extra miles on the tire treads” and give the injured joint a longer life. Damaged joint surfaces continue to wear down and become more and more damaged. Eventually artificial surface material must be inserted into the knee, such as metal and plastic to relieve pain. These artificial joints (total knee arthroplasty) can last 10-15 years or so. I try and delay these irreversible surgical procedures until later in life, say 55-60 years old. In that sense I am a “middle reliever” in baseball terms and the artificial metal and plastic joint is provided by the closing relief pitcher.
SURGICAL OPTIONS FOR BIOLOGIC RESURFACING OF LOCALIZED CARTILAGE DEFECTS:
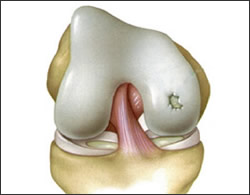
Figure 2 – Localized Cartilage Defects
1. Simple Arthroscopic Debridement
- During arthroscopy, shavers and rotating burrs smooth the cartilage surface and roughen the underlying bone to bring forth a fibro-cartilage biologic resurfacing response (abrasion arthroplasty).
- Crutches used for 4-8 weeks.
- Not the best over time.
- Benefits Uncertain.

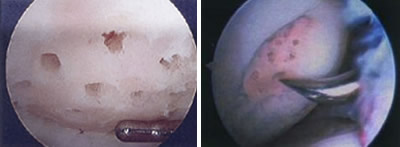
Microfracture Technique
2. Microfracture Technique
- Arthroscopic instrument is used to make simple holes in the bone after cartilage edges are smoothed. Commonly done.
- Long-term benefits not proven scientifically but this is surgically easy to do and less involved for the patient. Crutches used for 4-8 weeks.
Mosiacplasty/OATS Procedure
3. Mosiacplasty/OATS Procedure
- Multiple circular plugs of normal cartilage and bone transplanted from other parts of knee into the local defect.
- Crutches 4-8 weeks afterward. More involved surgery with inconsistent results reported in the literature. This is a reasonable alternative.
- More involved, often staged procedure as these fresh cadaver grafts must be sized from limited national supply.
- Insurance issues/payments are cumbersome.
- Safety issues are less of a problem now as tissue banks check on donors and make sure these transplant (cadaver) grafts are safe. FDA monitors the tissue banks.
- Crutches for up to 3-4 months afterwards to allow the transplant to biologically incorporate into your knee.
- 20-30% failure with collapse of graft .
- Biologic “rejection” is not a problem seen with transplanted organs.
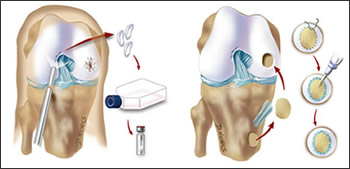
5. Autologous Chondrocyte Implant (ACI)
- Safe and well researched.
- 2 stage procedure where cells are taken from a safe area of your knee (about the size of 2 Tic Tacs), sent to Boston and stored frozen. With insurance clearance your cells are grown in a lab for 3 weeks and flown back to L.A. We then go back into a second surgery and insert 12-20 million of your grown cartilage cells into the knee defect and cover them with a patch of tissue.
- Crutches 4-8 weeks
- Proven decrease in pain and long-term follow-up reported up to 10 years.
Procedure
All of these procedures are attempts to biologically resurface your knee defect and hopefully “buy time” and keep you active and as pain-free as possible. Generally these resurfacing techniques are more involved and complicated surgical procedures.