Shoulder Instability
OVERVIEW / ANATOMY | SIGNS AND SYMPTOMS | DIAGNOSIS | TREATMENT | FREQUENTLY ASKED QUESTIONS
OVERVIEW / ANATOMY
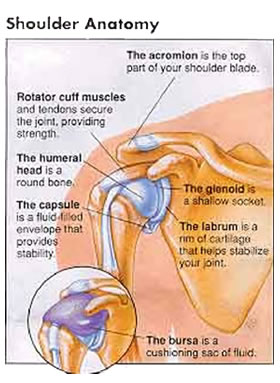
Figure 1 – Shoulder Anatomy
Unlike the hip, which is a “ball and socket” joint, the shoulder joint is less of a socket and looks more like a “golf ball on a tee”, allowing it to move more than any other joint in the body. It is this mobility that lends itself to potential instability.Your upper arm bone (humerus) acts as the “golf ball” on the “tee” (glenoid) (fig. 1). The glenoid is actually part of your shoulder blade. The glenoid has a rim of cartilage around it to help deepen the joint. This rim of cartilage is called the labrum. Covering the whole joint is the joint capsule, which is like a bag of flexible tissue that surrounds the joint. All of these components add structural stability to the shoulder joint.
Because the glenoid socket is very shallow, most of its stability comes from the ligaments, capsule and the four muscles that surround it, known collectively as the “rotator cuff”. The biceps also adds some muscular stability as it goes down a groove in the front of the upper arm bone (humerus).
The “bursa” is a cushioning fluid structure that lies between the top of the humerus and the tip of the shoulder (acromion) (fig. 2). Sometimes this structure can become compressed and inflamed leading to a painful “bursitis” condition called impingement.
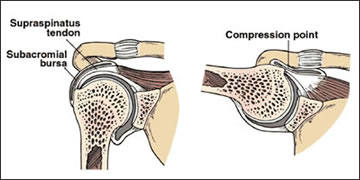
Figure 2 – Impingement of Bursa
Usually due to traumatic circumstances, the shoulder can become dislocated. This means that the humeral head has come out of the glenoid. Sometimes it reduces and returns to the usual golf ball on a tee position and sometimes it stays out of socket in the painful dislocated position. It can be relocated while the patient is awake, but sometimes reduction of a dislocation has to take place under anesthesia because the muscles that surround the shoulder become so tight (spasm). The most common direction for the humeral head to slip out is forward (anteriorly) and down.If the humeral head slides out of the socket partially and slides back in without completely dislocating this is called subluxation. Many structures, including the labrum can be injured when this happens.
Both dislocation and subluxation can cause the ligaments, capsule, and the labrum to become injured and create instability and pain. Patients may not be able to do certain activities because they have uncomfortable sensations and are afraid their shoulder will slip out of joint if they move their arm into certain positions. This is a particularly big problem for people who work with their hands above their heads or are “overhead athletes” like baseball pitchers and tennis players who depend upon their shoulder to play sports. These damaged tissues often don’t heal properly and the shoulder can develop recurrent painful dislocations/subluxations with certain types of activities. There is also a concern that the surface cartilage of the shoulder can be damaged if it slips in and out of joint frequently.
SIGNS AND SYMPTOMS
Dislocations of the shoulder are usually quite obvious as there is usually a traumatic event. Subluxations can develop with repetitive motions common to some sports. The patient usually has the following signs and symptoms:
- Pain
- Numbness/tingling of the involved arm and hand
- Loss of the normal contour of the shoulder
- Decreased ability/weakness to use the involved arm (“dead arm”)
- Instability
DIAGNOSIS
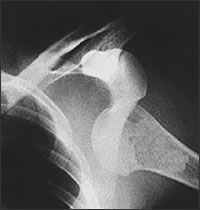
Figure 3 – X-Ray showing dislocated shoulder
I make the diagnosis of a dislocated shoulder by the combination of the history of injury, signs and symptoms on physical exam, and by x-rays that show that the humeral head is out of the socket (Fig. 3). The diagnosis of subluxation is made the same way, but the humeral head will still be in the socket because it has not completely dislocated. Occasionally I will get an MRI to look at these injured soft tissues.After the shoulder has been put back in the socket, the severe pain will stop almost immediately. The structures such as the labrum, bone, nerves, or ligaments were injured must be evaluated. The treatment that follows depends on what structures were injured, how many dislocations you have had, how unstable the shoulder is and how much pain you have. I most often immobilize the shoulder in a sling or sling and side pillow for a few weeks while the injury heals.
TREATMENT
Conservative nonoperative treatment including physical therapy to strengthen the muscles around the shoulder (rotator cuff) is best after the first dislocation. If you have had multiple dislocations or subluxations, I may suggest surgery to repair or tighten the capsule and ligaments that hold the shoulder in place. If the labrum has been injured, it will need to be trimmed or sutured. The surgery is usually done arthoscopically, which is less invasive and offers quicker return to full activity. The surgery is performed with a miniature lighted telescope (arthroscope) and small instruments introduced into the shoulder joint through hollow cannulas. Miniature anchors (screws) with suture attached are inserted precisely into the socket edge of the shoulder, and the torn ligaments and labrum are reattached to the socket. Complete healing from this procedure takes approximately 4-6 months.
The older a patient is at the time of dislocation the lower the chances are for developing recurrent dislocations. Patients over 35-40 can tear the rotator cuff with a dislocation. Patients under the age of 25 with traumatic dislocations have a substantially higher rate of recurrence (greater than 80-90%).
FREQUENTLY ASKED QUESTIONS
Click Here to view Frequently Asked Questions for Shoulder Instability / Impingement / Bursitis