What Happens When You Tear Your ACL?
Your anterior cruciate ligament, commonly known as the ACL, is one of the most important ligaments in your knee. Ligaments are vital components of movement because they stabilize joints. A problem in the ACL affects your ability to properly move and rotate the knee. Since it is also under the most stress, the ACL is one of the most commonly injured ligaments; over 200,000 people in the U.S. experience an ACL injury every year.
What Causes an ACL Tear?
 ACL tears are often seen in athletes, but they can occur for a number of reasons. Most ACL tears occur during sports, fitness activities, and other instances when stress is placed on the knee. Most people tear their ACL doing one of the following:
ACL tears are often seen in athletes, but they can occur for a number of reasons. Most ACL tears occur during sports, fitness activities, and other instances when stress is placed on the knee. Most people tear their ACL doing one of the following:
- Abruptly slowing and changing directions
- Pivoting with the foot firmly planted
- Landing from a jump incorrectly
- Stopping suddenly
- Collision or blow to the knee
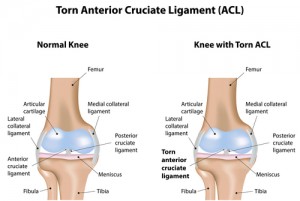
What Is an ACL Tear?
A tear in the ACL is exactly what it sounds like. The sudden shifting of the ligament causes a tear in the fibrous tissues. An untreated ACL tear can lead to serious long-term effects and damage to other functions of knee. This creates problems in the future.
Symptoms of an ACL Tear
- A “popping” sensation in the knee
- Severe pain around the knee
- Swelling
- Loss of motion
- Inability to bear weight on the affected leg
Treating an ACL Tear
If you believe you have torn your ACL, it is important to see a doctor immediately for diagnosis. A physical test is performed to check the integrity of the ACL, and an MRI may be performed to confirm the diagnosis of an ACL tear. After diagnosis, an ACL tear is treated as soon as possible to minimize the possible long-term effects.
Non-Surgical Treatments
Your orthopedic surgeon will determine if surgery is the best option at the time. However, whether or not you are undergoing surgery, non-surgical treatments help ease pain and increase the strength of your knee.
- Attempt to decrease swelling using the RICE technique (rest, ice, compression, elevation)
- Perform small exercises to regain full range of motion of the knee joint
- Increase the strength of the muscles surrounding the knee
Surgery
Patients with a torn ACL who are active in sports or have recurrent instability episodes should consider surgery. ACL reconstruction is an outpatient procedure that removes the torn ligament and grafts a new ligament with your own tissue or donor tissue.
- Autografts use your own tissue. The surgeon must cut into the bone, which may result in a more painful and longer recovery.
- Allografts use tissue harvested from a donor or a cadaver that has been thoroughly screened for diseases so there is no chance of infection. The advantage of an allograft is that your body only has to heal the new ligament site and not the graft site.
Following your surgery, the knee is kept straight. Physical therapy in the weeks following your surgery will help you regain strength initially and range of motion in the knee. With proper care and physical therapy, you may be able to return to sports six to nine months after your surgery.
Long-Term Effects of ACL Reconstruction
Patients with a torn ACL, reconstructed or not, are more likely to experience knee cartilage damage over time. However, patients who didn’t undergo reconstruction surgery were five to six times more likely to experience cartilage degeneration at an increased rate. ACL reconstruction after a tear protects the meniscus and protects patients from developing osteoarthritis over time.
The ability to return to high-intensity pivoting sports and other physical activities will vary depending on the severity of your initial injury and your recovery process. Treating a torn ACL as soon as possible and properly following your postoperative physical therapy will increase your chances of being able to return to your regular activities.
Dr. Vangsness is a leading senior orthopedic surgeon at USC. If you need an ACL reconstruction consultation or have any questions about a previous ACL surgery, schedule your consultation today. Call us at (323) 442-5800 or contact us online.
Placenta-Derived Products
Numerous products exist that utilize placental tissue that would be otherwise discarded. These products are primarily delivered via injection. Placenta-derived tissues include: the amniotic membrane, the chorionic membrane, the amniotic fluid, the umbilical cord, and the blood from the umbilical cord. Placenta-derived products are composed of one or more of these tissue types and/or the matrix secreted by any of these cells. Placenta-derived products have commonly been used in ligament and tendon injuries of the foot and ankle, but they have also been used for conditions like knee osteoarthritis. They are thought to have regenerative properties, though this has yet to be proven. Placenta-derived products are not covered by insurance or Medicare.
Bone Marrow Aspirate Concentrate (BMA/BMAC)
Bone marrow aspirate concentrate (BMA/BMAC) is perhaps the most popular “stem cell injection” available today. The treatment involves injecting the patient’s own bone marrow cells into the injured area with the hope that it will help regrow tissue or reduce inflammation. The procedure involves two steps: (1) patients are lightly anesthetized and bone marrow is removed through a needle from the bone, most commonly the iliac crest of the patient’s hip, and then (2) the bone marrow is processed to concentrate the cells. After the bone marrow has been centrifuged (spun in a circle to separate the various blood contents), the BMA/BMAC is put into a syringe and injected into the affected body part.
Bone marrow contains progenitor cells, which are cells that have been “primed” to become specific cells. A small fraction of these cells (about 1% of the total cells in bone marrow) are mesenchymal stem cells, which can become cartilage, bone, and tendon cells. It is thought that these mesenchymal progenitor cells release chemicals that decrease inflammation and help regenerate tissue and other structures in degenerative conditions like knee osteoarthritis and rotator cuff tears.
Studies have shown that BMA/BMAC injections may be successful in relieving pain and improving function for various orthopaedic conditions, including osteoarthritis, tendon injuries and certain spine conditions. We still do not know exactly how these cells function after being injected into the body. BMA/BMAC injections are not covered by insurance or Medicare.
Choosing an Orthopedic Surgeon
When joint problems escalate to the point of needing special treatment, it is time to research orthopedic surgeons. As you consider your treatment options, it is important to choose an orthopedic surgeon who can accurately meet your needs. To ensure that you make the best choice, identify your needs, do your research, and ask the right questions.
 Identify Your Needs
Identify Your Needs
Before you seek out a surgeon to help you, identify and become completely clear on what your needs are for orthopedic treatment. Determine your goals: are you seeking relief from everyday pain or are you hoping to be able to engage in strenuous physical activities? Decide whether you are interested in a specific technique or procedure or whether you are interested in participating in a clinical trial or innovative treatments. Bear in mind that orthopedic surgeons located in larger cities may be more likely to have the experience, equipment, and medical staff to perform certain specialized procedures. You should also consider your logistical and financial needs, such as what your insurance plan will cover and if there are any restrictions in your choice of physician, surgical facility, or rehabilitation center. Identify any other limitations that could affect your decision, including your travel radius and transportation resources. These factors could affect not only your treatment itself but the lengthy recovery period as well.
Do Your Research
To find the best surgeon for your needs, do your research. Be informed about all the treatment options for your needs. You will quickly learn that even within the field of orthopedic surgery, not every surgeon performs the same treatments. Most surgeons specialize in a few specific areas, and you will want to select a surgeon within your travel radius who specializes in what you need. Most will have detailed information regarding their expertise, specializations, credentials, training, and experience on their websites or at their offices.
Ask the Right Questions
Once you’ve narrowed down your pool of potential orthopedic surgeons, ask each of them the following questions:
- Do you perform my desired treatment?
- What would be your recommended treatment for my condition and why?
- How often do you perform this particular treatment? How many times have you performed this treatment in the past year?
- Do you prefer to practice innovative techniques or traditional time-proven procedures? What are your reasons for doing so?
- What is your complication rate?
- What will my follow-up care include?
- How will your medical team help me before and after my procedure?
You should also ask any other questions that come to mind. As the surgeon answers all your questions, determine how you feel about the responses. If you feel comfortable working with this surgeon, your communication is strong, and the surgeon will be able to help you in the ways that you need, you can feel confident moving forward with that orthopedic surgeon.
C. Thomas Vangsness Jr., MD, is a board-certified orthopedic surgeon who specializes in the treatment of sports injuries. Dr. Vangsness also specializes in performing rotator cuff surgery and torn ACL repair as well as other orthopedic surgeries and minimally invasive techniques for cartilage repair, meniscus surgery, shoulder instability, and more. To schedule your consultation with Dr. Vangsness, call (323) 442-5800 today or contact us online at your convenience.
Hyaluronic Acid (HA) Injections
These injections are used to treat knee osteoarthritis. Hyaluronic acid is naturally found in your body as a part of healthy synovial fluid (the substance that lubricates joints). Injecting HA into the knees of patients with osteoarthritis is thought to help lubricate the joint, which reduces catching and grinding. Research suggests that HA injections may also help reduce inflammation. Treatment is often offered in a series of three to five injections one week apart, but some brands only require one injection.
There are 9 types of HA injections that have been FDA-approved to treat knee osteoarthritis in the United States: Hyalgan®, Supartz®, Orthovisc®, Monovisc®, GEL-SYN®, Synvisc(-One)®, Euflexxa®, Gel-One®, and GenVisc 850®. No HA product has been proven to work better than the others. However, each person is different and some patients respond better to a particular type of HA injection. Most insurance plans will cover one of the preceding HA treatments (single injection or multiple injections, depending on the brand) every six months.